KPV Peptide Benefits: Expert Guide You Need Today
The peptide KPV (Lys-Pro-Val) has shown remarkable anti-inflammatory properties in preclinical studies. Unlike traditional nonsteroidal anti-inflammatory drugs that can cause gastrointestinal irritation or cardiovascular complications, KPV operates by modulating the immune response at a cellular level. In laboratory models of asthma, arthritis, and inflammatory bowel disease, administration of KPV led to a marked reduction in pro-inflammatory cytokines such as tumor necrosis factor alpha and interleukin-6. Moreover, KPV appears to enhance mucosal barrier function, which is particularly valuable for gastrointestinal disorders where epithelial integrity is compromised. The peptide’s short amino acid sequence allows for relatively straightforward synthesis, potentially reducing production costs compared with larger biologic agents. Additionally, because KPV targets specific inflammatory pathways rather than broadly suppressing the immune system, it may offer a safer profile for long-term use.
Part 1. What Is KPV Peptide?
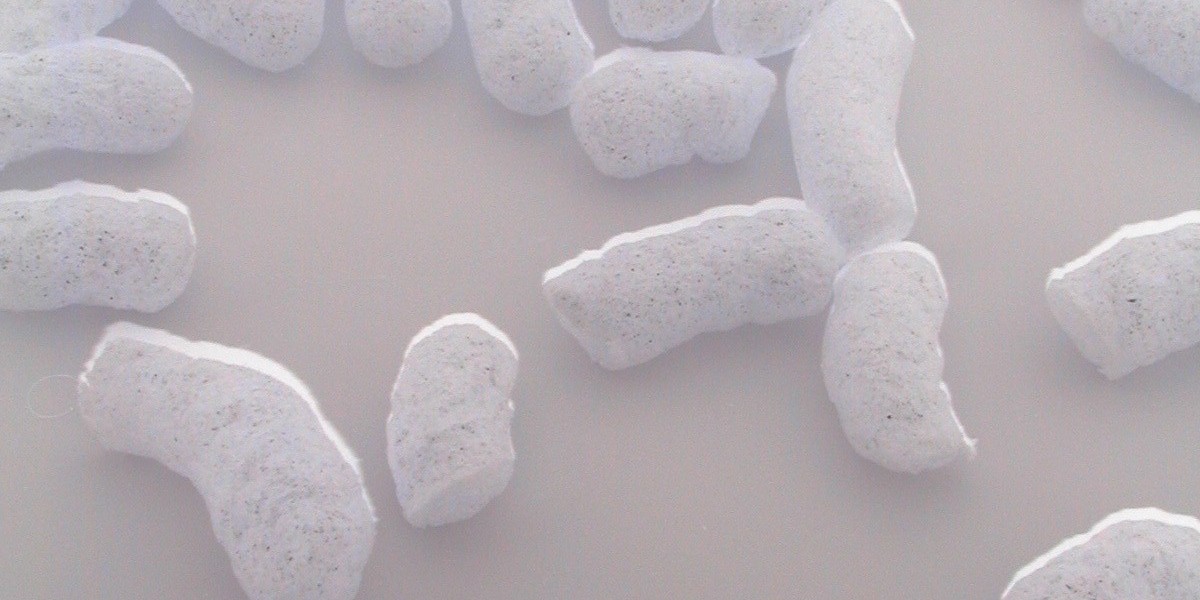
KPV is a tripeptide composed of lysine, proline, www.fionapremium.com and valine residues arranged in that order. Its sequence confers stability against proteolytic enzymes, allowing it to persist longer within tissues than many other short peptides. The mechanism by which KPV exerts its effects involves interaction with the formyl peptide receptor family on immune cells. By binding to these receptors, KPV inhibits neutrophil migration and degranulation, thereby dampening acute inflammatory responses. In addition, studies suggest that KPV can induce apoptosis in activated T-cells, further contributing to its anti-inflammatory action. Because of its small size, KPV is amenable to various delivery routes, including topical formulations for skin inflammation and inhalation therapies for respiratory conditions.
The Problem With KPV
Despite promising data, several challenges remain before KPV can be widely adopted in clinical practice. First, most evidence comes from animal models; human trials are still scarce, leaving uncertainty about efficacy and safety in diverse patient populations. Second, the peptide’s stability outside controlled laboratory settings is limited; exposure to body fluids or environmental conditions can degrade it, potentially reducing therapeutic potency. Third, while KPV targets inflammatory pathways, its precise selectivity profile has not been fully mapped; off-target effects could arise when administered at higher doses or over prolonged periods. Finally, regulatory approval processes for peptide therapeutics are rigorous, requiring extensive pharmacokinetic and toxicological studies that can be costly and time-consuming. Addressing these issues will require coordinated research efforts, including well-designed clinical trials and the development of robust delivery systems to ensure consistent bioavailability.
In summary, KPV peptide represents an exciting frontier in anti-inflammatory therapy, offering targeted modulation of immune responses with a potentially favorable safety profile. Understanding its mechanism, benefits, and current limitations is crucial for researchers, clinicians, and patients who are considering this novel approach as part of a broader strategy to manage chronic inflammatory diseases.